The New Implementation of Electronic Scripts in South Africa
- by Mamparra

Prescription medications in South Africa should be written in legible print, typed, or computer generated and signed in person by a licensed prescriber by the overall legislation established as a result of the Medicines and Related Substances Act. Amidst these regulations, prescribers regularly encounter handwritten prescriptions that are difficult to read, increasing the likelihood of medication mistakes.
Medication errors are responsible for the deaths of 7,000 people per year in the United States and contribute to nearly one in twenty hospitalizations. These errors can be caused by things like sloppy handwriting, client allergies, incorrect dosages, and drug reactions. Comparable safety concerns exist despite the lack of available SA data.
Electronic prescriptions have been incorporated in countries like the United States to address the shortcomings of paper prescriptions, and their use has increased by 72% between 2009 and 2010. Denmark, Estonia, Iceland, Sweden, Norway, The Netherlands, Greece, England, Scotland, Wales, and Northern Ireland are just some of the other countries that have implemented e-prescribing. E-prescribing pilot programs are active in the Czech Republic, Finland, Italy, and Poland at present. The transition to e-prescribing has officially started in South Africa. With the help of e-prescribing, doctors at the point of treatment can instantly and accurately transmit prescriptions to local pharmacies over the internet.
Nevertheless, electronic prescribing refers to more than just writing a script on a computer. To have a fully functional e-prescribing system, you need things like a back-end operating system, automated dispensing records, automatons, automated drugstore processes, bar coding, digital release prescriptions, and specific patient data. To put it simply, an electronic prescribing system is a digital version of a traditional medical reference book. The most advanced electronic prescribing tools can even function independently as prescription generators. Personal prescriptions can be written and refilled, medications and patient records accessed, a link established to a pharmacy or other drug distribution facility, and communication with the digital rendition of the South African Medicines Formulary (SAMF). Electronic prescribing (or “e-prescribing”) is the process by which a prescription is written on a computer, checked with an e-signature, filed or transmitted electronically, and filled at a pharmacy.
Regulations About Digital Scripts
On August 30, 2002, the Electronic Communications and Transactions Act (ECT Act) became law. This Act’s stated purpose is to promote the use of electronic communication and commerce for the benefit of all parties involved. Electronic prescriptions in South Africa are governed by the ECT Act, which must be read in conjunction with the Medicines and Related Substances Act.
Data that is transmitted entirely or partially in the form of a data message does not lose its legal force and effect, as guaranteed by the ECT Act. Therefore, a computer-generated prescription might be treated the same as any other prescription. A data message that can be retrieved in a way that is usable for future reference satisfies the necessity that a prescription is in written form. Electronic signatures attached to the script are valid and binding under the law regardless of the medium in which they are transmitted. Until proven otherwise, a modern automation signature is considered to be a legitimate digital signature when used correctly.
Within 7 working days of receiving a prescription or order via fax, email, telephone, or electronic means in South Africa, the original document must be presented. If electronic prescriptions have the same legal force as written prescriptions, then it is unclear if this necessity will apply to them. The addressee of a data message is the individual who is the intended recipient of the message from the sender but does not include any intermediaries. Therefore, it is crucial that a licensed prescriber, with the patient’s permission, transmits a prescription data message to a preferred pharmacy. No professional pharmacist would ever discourage a patient from picking their pharmacy.
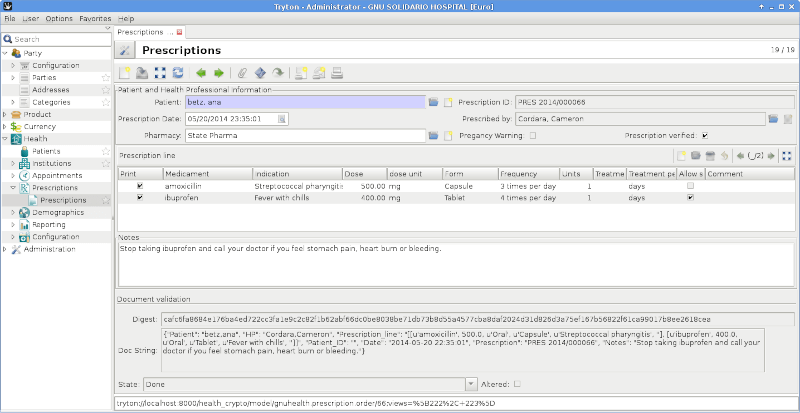
Prescriptions can now be sent and received electronically, but this requires that proper protocols be in place to ensure the security of the transmitted data. Practitioners are tasked with determining whether or not an electronic prescription is legitimate. They should be familiar with common techniques used to fake prescriptions and use caution when doing so. Several methods exist for this, including the use of passwords, PINs, and other forms of authentication in software.
The pharmacist may be alerted by some programs if the text has been changed. The physician is responsible for determining whether or not the data in a digital prescription has been altered beyond the addition of approval and the changes that would occur during the regular course of storage and transmission. If the patient keeps the “original” prescription or requests to use a separate pharmacy, the e-script could be confirmed by a product code on the e-script that is identified by all the various distributing software applications to allow monitoring of the prescription’s history.
In SA, it is required that a hard copy of any prescription or order that is faxed, emailed, telephonically, or otherwise transmitted electronically be made and kept on file. Any changes to the prescription, such as a request for a generic alternative or a note from the prescriber indicating that the medication should not be dispensed, must be noted on the back of the prescription. It is recommended that prescriptions be kept for 5 years. This same treatment is required for an electronic script.
The confidentiality and privacy of patients must be maintained throughout the process of gathering, recording, and using their health data. Consequently, prescribers and pharmacists need a secure network for digital communication, and the hardware utilized must be kept in safe facilities. No intermediaries may be used for transmissions. Remember that without the patient’s consent, it’s not a good idea for a doctor to email a prescription to a pharmacy because it does not protect patient privacy.
The Pros and Cons of Electronic Scripts
Patient safety and care quality are both enhanced by the use of electronic prescriptions, which eliminate the need for manual scripting and subsequent phone calls to pharmacies to clarify or clarify information. Because of the e-prescribing system, all the necessary and specific data for filling a prescription is made available. Potentially helpful in preventing adverse drug effects are warning and alert systems implemented at the point of care.
The Pros
The system also helps doctors and pharmacies follow the patient’s insurance or health plan’s formulary more closely, which means cheaper drugs can be used instead. In addition, patients have the option of submitting prescription renewal requests electronically. E-prescribing systems provide clinicians with several benefits, including the ability to more easily and securely organize their patients’ medication regimens and the flexibility to prescribe from anywhere. Patients will spend less time waiting in line at the pharmacy, and pharmacists will be able to increase their productivity and patient care through enhanced patient counseling and professional service if prescriptions are downloaded electronically. However, there are some drawbacks to electronic scripts as well.
The Cons
These include the high price tag associated with acquiring, launching, and maintaining an e-prescribing platform, in addition to the time and money needed to train staff. Disruptions to the system could be annoying. Mistakes that lead to the accidental disclosure of online health information pose a risk to the safety and confidentiality of patients’ information.
Plus, modern technology facilitates the process of forging and altering prescriptions. South Africa faces difficulties such as meeting the demand for electronic scripts in our 11 official languages. It may be difficult to avoid typos and keep track of correct packaging sizes and doses. Electronic scripts incorporate ICD-10 codes, but some patients may feel awkward discussing their medical histories in this public forum. Manual labor is frequently required to complete the automated repeat storage process. It may be expensive, but it is necessary to train all employees, including temporary ones.
Conclusion
Improved patient safety, ease for the doctor, and time savings at the pharmacy are just a few of the benefits of electronic prescriptions. Electronic scripts have many benefits, but the implementation process can be challenging. E-prescribing would be much more practical for the patient. Automatic prescription renewals will never be able to replace the need for regular check-ins with a doctor to monitor the progress of chronic conditions. Click here for more information and assistance.
Prescription medications in South Africa should be written in legible print, typed, or computer generated and signed in person by a licensed prescriber by the overall legislation established as a result of the Medicines and Related Substances Act. Amidst these regulations, prescribers regularly encounter handwritten prescriptions that are difficult to read, increasing the likelihood of…
Recent Mamparras
- The Accidental Aboriginal’s Legacy
- The Origins of Oktoberfest
- Fascinating Quick Facts
- Insect Winter Hideaways Decoded
- Decoding the Pharaohs’ Secret Language
- The Geological Marvel of Himalayan Formation
- Hetty Green – The Frugal Financial Genius
- Split Brain Syndrome
- Mosquito-Borne Cancer Pandemics
- Entertainment’s Sweet Surprise – Women in Cakes
- Lighting the Trenches With Glow Worm Tactics
